Orthostatic hypotension is a type of low blood pressure. This occurs once the blood vessels do not tighten when standing up. It is usually an indication of an underlying condition.
When standing up from a seated or lying down position, the blood vessels react to gravity by narrowing to prevent the blood pressure from dropping. This guarantees a constant supply of oxygenated blood to the brain. Most are likely to experience a mild form at some time. It is usually a lightheaded sensation when getting out of bed quickly.
What are the indications?
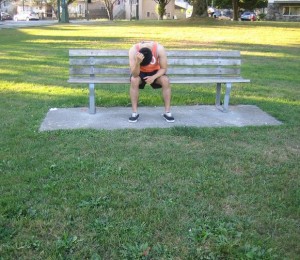
A drop in the blood pressure lowers the flow of oxygenated blood to the brain. The usual symptoms include the following:
- Lightheadedness
Drink more fluids throughout the day to prevent dehydration. - Blurred vision
- Nausea
- Dizziness
- Muscle tremors
- Fainting
- Mental confusion
What are the causes?
Orthostatic hypotension is usually brought about by an underlying health condition. Some of the usual causes include the following:
- Fever
- Excessive consumption of alcohol
- Extended bed rest
- Dehydration due to diarrhea, vomiting or both
- Using certain medications such as antihypertensive medications or diuretics
- Heart issues including erratic heartbeat, aortic stenosis, congestive heart failure or heart attack
- Nervous system conditions such as neuropathy or Parkinson’s disease
- Extensive blood loss
- Spinal cord conditions
Management of orthostatic hypotension
The treatment is usually based on the cause. The commonly used options include the following:
- Administration of fluids to manage dehydration
- Regular insulin injections to manage diabetes
- Altering the dosage in medications if they are the cause
- Medications, surgery or both to manage heart conditions
- Medications to increase the blood volume or pressure
Self-care measures
The general recommendations that can help manage orthostatic hypotension include the following:
- Raise the head using pillows while in bed to reduce the likelihood of orthostatic hypotension upon getting up.
- Move slowly from a seated or lying position to allow the blood vessels enough time to adjust.
- Eat small, frequent meals instead of 3 large meals per day.
- Use support stockings to minimize the pooling of blood in the legs to improve the blood pressure.
- Drink more fluids throughout the day to prevent dehydration.
- Reduce the consumption of alcohol since it increases the risk of dehydration and dilation of the blood vessels.
- Lower the intake of caffeine to small but regular doses to boost the blood pressure.
- Avoid engaging in strenuous exercise, saunas, hot baths and any hot environments since it widens the blood vessels.
- Avoid ascending quickly to high altitudes.
- As much as possible, avoid standing without moving for long periods of time.
- Consult a doctor for regular blood pressure monitoring.